
You're on your way!
You're being directed to a third-party site to get a quote.
Since 2011, we've helped more than 5 million visitors understand Medicare coverage.
By shopping with third-party insurance agencies, you may be contacted by a licensed insurance agent from an independent agency that is not connected with or endorsed by the federal Medicare program.
These agents/agencies may not offer every plan available in your area. Please contact Medicare.gov or 1-800-Medicare to get information on all options available.
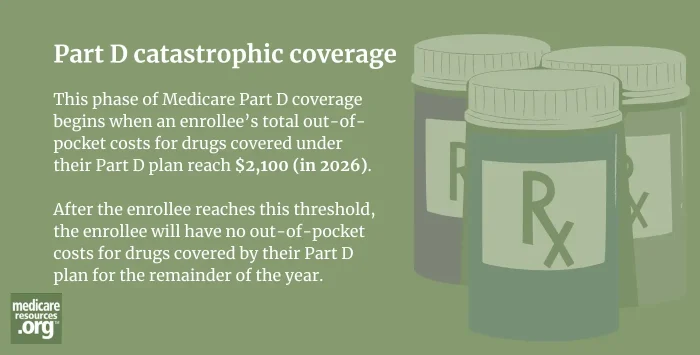
Catastrophic coverage is the phase of Medicare Part D coverage during which an enrollee’s covered drugs no longer have any out-of-pocket costs for the remainder of the year. Instead, the costs are paid by the drug manufacturer, Medicare, and the Part D plan.1
The elimination of out-of-pocket costs during the catastrophic coverage phase took effect in 2024, due to the Inflation Reduction Act. And that law further limited Part D out-of-pocket costs starting in 2025. Before 2024, enrollees had unlimited out-of-pocket costs during the Part D catastrophic coverage phase.
Historically, there were four phases of Part D coverage: The deductible phase, the initial coverage phase, the coverage gap (donut hole) phase, and the catastrophic coverage phase.2 But starting in 2025, the coverage gap phase was eliminated, due to the Inflation Reduction Act. And out-of-pocket costs have been simplified and reduced. Here’s how the Part D coverage phases work in 2026:3
Footnotes