
You're on your way!
You're being directed to a third-party site to get a quote.
Since 2011, we've helped more than 5 million visitors understand Medicare coverage.
By shopping with third-party insurance agencies, you may be contacted by a licensed insurance agent from an independent agency that is not connected with or endorsed by the federal Medicare program.
These agents/agencies may not offer every plan available in your area. Please contact Medicare.gov or 1-800-Medicare to get information on all options available.
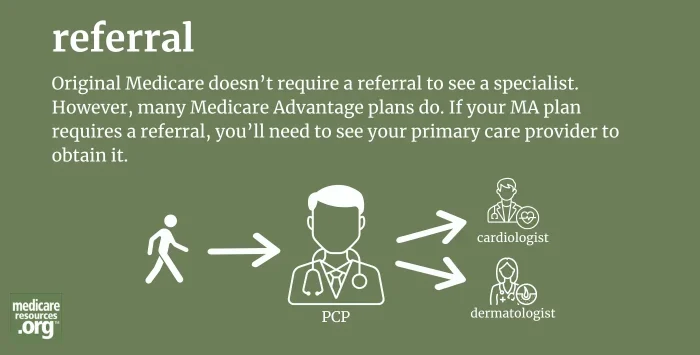
When one medical provider formally sends a patient to see another medical provider for further evaluation or treatment, this is called a referral. It’s common for primary care providers (PCPs) to refer their patients to specialists (for example, an orthopedist, oncologist, or cardiologist) so that they can obtain a diagnosis or receive care for a particular medical condition.
Many health plans require their members to get a referral from a PCP before the plan will cover specialty care.
Original Medicare (Parts A and B) does not require referrals. You can see any medical provider, including specialists, as long as they accept Medicare, and you don’t need to get a referral to do so.1
However, many Medicare Advantage plans do require referrals before a member can see a medical specialist. This includes Medicare Advantage HMOs (health maintenance organizations) and POS (point of service) plans.
If you have a PPO Medicare Advantage plan, you will not likely need a referral to see a doctor other than your primary care doctor. But if your Medicare Advantage plan is an HMO or a POS, you’ll likely need a referral.
If your Medicare Advantage plan requires referrals, you’ll need to first schedule a visit with your PCP before visiting a specialist, so that you can obtain the necessary referral.
Footnotes