
You're on your way!
You're being directed to a third-party site to get a quote.
Since 2011, we've helped more than 5 million visitors understand Medicare coverage.
By shopping with third-party insurance agencies, you may be contacted by a licensed insurance agent from an independent agency that is not connected with or endorsed by the federal Medicare program.
These agents/agencies may not offer every plan available in your area. Please contact Medicare.gov or 1-800-Medicare to get information on all options available.
Update, April 7, 2025: In November 2024, CMS proposed a rule change that would have allowed Medicare Part D to cover drugs prescribed for weight loss to treat obesity, starting in 2026.1 But in April 2025, when the final rule was published, CMS noted that they had decided not to finalize that portion of the proposed rule.2 So nothing has changed about Medicare Part D coverage of GLP-1 drugs: They continue to only be covered if they’re prescribed to treat another condition, like diabetes, but not if they’re prescribed just to treat obesity.
If a prescription drug is being used for weight loss rather than to treat another medical condition, Medicare Part D (Medicare prescription coverage) will not cover the drug. But if the drug is prescribed to treat another medical condition – such as type 2 diabetes – it can be covered by Medicare Part D.
Under long-standing federal rules, medications “used for anorexia, weight loss, or weight gain, are specifically excluded from the definition of Part D drugs.”3
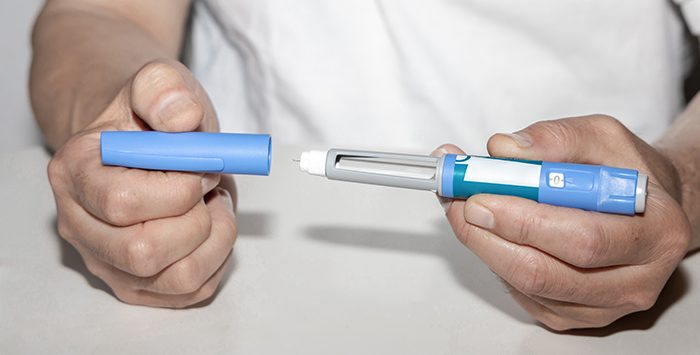
But glucagon-like peptide-1 (GLP-1) receptor agonists such as Ozempic and Mounjaro can be covered by Medicare Part D if they’re prescribed for other medical conditions.4
(Note: If a Part D plan is an “enhanced alternative coverage” plan, drugs that would otherwise have to be excluded, including medication to treat obesity, can be covered by the plan as supplemental drugs.5 The full premium cost for the coverage of the supplemental drugs is paid by the enrollee, and is not subsidized by Medicare.6 But enhanced alternative coverage plans are not required to cover weight-loss medications.)
Most GLP-1 drugs have FDA approval to treat type 2 diabetes.7 And Wegovy was recently given FDA approval to reduce the risk of serious cardiovascular events in adults who have cardiovascular disease in addition to obesity or overweight.8 As a result, Wegovy for those patients can be covered by Medicare Part D.9
CMS added clarity to this topic in a March 20, 2024 memo.4 The agency reiterated the fact that Medicare Part D cannot cover medications used for weight management. But CMS noted that the same medications can be covered by Medicare Part D if they’re prescribed to treat another medical condition:
“For example, a glucagon-like peptide 1 (GLP-1) receptor agonist that receives FDA approval for chronic weight management alone would not be considered a Part D drug. If this same drug also receives FDA approval to treat diabetes or reduce the risk of major adverse cardiovascular events (cardiovascular death, non-fatal myocardial infarction, or non-fatal stroke) in adults with established cardiovascular disease and either obesity or overweight, then it would be considered a Part D drug for those specific uses only”
If you’re prescribed a GLP-1 for type 2 diabetes or cardiovascular risk reduction, your out-of-pocket costs will depend on the specific drug and your Medicare Part D coverage details, including whether your plan has that particular drug on its formulary (covered drug list).
Your out-of-pocket costs will also depend on whether you’ve already met your Medicare Part D deductible (if your plan has one), and whether you’ve reached the coverage gap.
You can use the Medicare plan finder tool to see how various plans in your area would cover GLP-1 drugs. As an example, we’ll consider plans in Illinois (using 60647 as the zip code) and look at coverage for Ozempic and Mounjaro.
First, let’s consider stand-alone Medicare Part D plans (PDPs) in the 60647 zip code (in the Illinois PDP region):10
Now let’s use the Medicare Plan finder tool to look at Medicare Advantage plans with integrated Part D coverage (MA-PDs), available in the Chicago, Illinois area (zip code 60647):
This illustrates how much variation there can be from one PDP or MA-PD to another, in terms of whether a given drug is covered and if so, how much it will cost to fill the prescription. These variations are a reminder of why it’s so important to carefully compare the available plan options each year during the annual Medicare open enrollment period.
If you’re enrolled in Medicare and discussing a GLP-1 with your doctor, you’ll want to make sure you understand your plan’s formulary and out-of-pocket costs, and include that in your conversations with your doctor.
Keep in mind that your Medicare Part D plan – either a PDP or an MA-PD – cannot provide any coverage for a GLP-1 if it’s prescribed for weight loss (unless it’s an enhanced alternative coverage plan, as described above). So even if your plan covers the drug you and your doctor are considering, that coverage will only be available if the medication is prescribed to treat a medical condition other than obesity or overweight.
And carriers are increasingly checking to make sure that the prescription isn’t for weight loss. Some major Medicare Advantage insurers have begun using a prior authorization process to make sure that they’re only covering GLP-1 drugs for patients who have been diagnosed with type 2 diabetes.5
There are no longer any out-of-pocket costs for covered drugs once a person gets out of the Medicare Part D coverage gap and enters the catastrophic coverage phase.12 But it’s important to note that this is only applicable insofar as the medication is covered by the PDP or MA-PD.13 If a particular drug isn’t covered, the beneficiary’s costs for those drugs will not accrue toward getting out of the coverage gap and there are no limits on how high the out-of-pocket costs can be.
There has been a sharp rise in GLP-1 prescriptions in recent years.14
Given that Medicare Part D does cover GLP-1 drugs when they’re prescribed for something other than weight loss, it’s not surprising to see that total Medicare Part D spending on these drugs has ballooned in recent years.
KFF recently reported that Medicare Part D spending on Ozempic was 81 times higher in 2022 than it had been in 2018 ($4.6 billion in 2022, versus $56.8 million in 2018).15
When we include Rybelsus and Mounjaro, total Medicare Part D spending across the three drugs was 100 times higher in 2022 than it had been in 2018.
Although most Medicare beneficiaries have drug coverage under Medicare Part D, more than 16% have another source of drug coverage – typically from a current or former employer, with or without the retiree drug subsidy program.16
If you’re enrolled in Medicare and your drug coverage is not provided via a PDP or MA-PD, the specifics of your coverage will depend on your plan. It might cover GLP-1 drugs when they’re prescribed for weight loss, as it wouldn’t have the same statutory prohibition that applies to Part D coverage.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written hundreds of opinions and educational pieces about the Affordable Care Act and Medicare for healthinsurance.org and medicareresources.org.
Footnotes