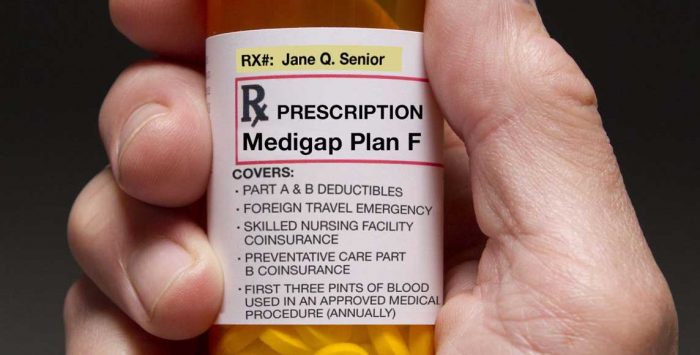
Is there a best time to enroll in a Medicare supplement (Medigap) plan?
A: Yes. The best time to enroll is during your Medigap open enrollment period, a six-month window of time that begins on the first day of the month that you are at least 65 years old and are enrolled in Medicare Part B (you must also be enrolled in Part A to buy a Medigap plan, but for people who enroll in Part A when they turn 65 but delay their enrollment in Part B, the Medigap open enrollment period begins once they enroll in Part B).
During this period, a private insurance company that offers Medigap coverage can not:
- refuse to sell you any Medigap policy it offers
- charge you additional fees for your coverage because of your medical history, or
- make you wait for coverage of pre-existing conditions to take effect (except under certain circumstances);
Even if you enroll during your initial enrollment period, a private Medigap insurer may refuse (for up to six months) to pay your out-of-pocket expenses for a pre-existing health issue. If your pre-existing condition was diagnosed or treated within six months before the date your Medigap supplemental coverage was to begin, the insurance company can make you wait up to six months before covering your out-of-pocket expenses for the pre-existing condition.
But if you had creditable coverage before enrolling in Medigap, without a gap in coverage of more than 63 days, the pre-existing condition waiting period will be reduced by the number of months that you had creditable coverage. So if you had continuous coverage for six or more months before enrolling in Medigap, you won’t have a pre-existing condition waiting period. The rules can be confusing, so don’t hesitate to talk to a representative of the Medigap insurance company for clarification.
Can I buy a Medigap plan after my enrollment initial window closes?
After your six-month open enrollment window, Medigap plans are medically underwritten in nearly every state, meaning that if you apply for coverage outside of your open enrollment window, you can be declined or charged more based on your medical history.
(States with exceptions to this rule are discussed below).
There are also some limited special enrollment periods for Medigap coverage, including
- Moving out of your Medicare Advantage plan’s service area
- Losing a group or retiree plan that has been paying secondary to Medicare
- Your Medigap or Medicare Advantage plan leaves Medicare or stops offering coverage in your area, or you leave the plan because it didn’t follow Medicare’s rules.
- You enrolled in a Medicare Advantage plan when you first became eligible for Medicare, and are utilizing your “trial right” to switch to Original Medicare within 12 months of purchasing the Medicare Advantage plan (this only applies the first time you join Medicare Advantage).
- You were previously enrolled in Original Medicare plus a Medigap plan, dropped them to enroll in Medicare Advantage, and decided within 12 months that you wanted to switch back. You’ll be limited to switching back to your original Medigap plan, unless it’s no longer available. In that case, you’ll be able to pick a different Medigap plan. But although people can switch back and forth between Original Medicare and Medicare Advantage every year, the option to have guaranteed-issue access to Medigap in this scenario is limited — it only applies the first time you’re switching back to your old Medigap plan, and only if you do so within 12 months of leaving the Medigap plan.
States with extended guaranteed issue for Medigap plans
- In New York and Connecticut, Medigap plans are not medically underwritten, regardless of when an applicant enrolls.
- In Massachusetts, there is an annual guaranteed-issue Medigap open enrollment period each year, from February 1 through March 31, during which Medicare beneficiaries can enroll in Medigap for the first time or switch to a different Medigap plan.
- In Maine, Medigap insurers must offer Plan A on a guaranteed issue basis for at least one month each year, regardless of the applicant’s medical history.
- Missouri‘s “anniversary rule” allows enrollees a guaranteed issue right to switch to another Medigap plan (the same letter plan from a different insurer) during a 30-day period each year preceding the anniversary of when their Medigap plan was purchased.
- California, Idaho, Illinois, Maryland, Oregon, Nevada, Louisiana, and Kentucky have “birthday rules” that allow Medigap enrollees a time-limited window each year, around their birthday, when they can switch (without medical underwriting) to another Medigap plan with the same or lesser benefits.
- Washington State allows Medigap enrollees to switch to a different Medigap plan at any time, as long as they’ve had coverage for at least 90 days. People with Medigap Plan A are limited to switching to only another Plan A. But people with Medigap Plans B through N can switch to any other Plan B through N.
- Several other states offer limited guaranteed issue rights for Medigap enrollees in certain circumstances, including states with “birthday rules” that provide the option to switch to a different Medigap policy (with limitations that vary by state) during an annual window around the enrollee’s birthday.
Can I make Medigap changes during Medicare's annual open enrollment period?
You can certainly apply for a new Medigap plan during the annual Medicare open enrollment period (October 15 to December 7). But that window is no different from any other time of the year when it comes to Medigap.
The annual Medicare open enrollment period (annual election period) is for Medicare Advantage and Part D plans, but it doesn’t change anything about the normal enrollment rules for Medigap. In most states, if your initial enrollment window has ended and you don’t qualify for a special enrollment period, Medigap insurers will use medical underwriting if you submit an application for a new plan, regardless of what time of year you apply.
So for example, if you want to use the annual open enrollment period to switch from Medicare Advantage to Original Medicare, you can do that. And you’ll be able to enroll in a stand-alone Part D plan to supplement your Original Medicare. You’ll be able to apply for a Medigap plan as well, but in most states, the coverage will not be guaranteed issue — your eligibility will depend on your medical history. (Note that if your Medicare Advantage plan is ending on Dec. 31 and thus not available for renewal, you will have guaranteed-issue access to most of the Medigap plans available in your area, if you choose to switch to Original Medicare instead of a different Medicare Advantage plan.)
The same will be true if you want to try to switch from one Medigap plan to another. Let’s say you have Original Medicare plus a Part D plan and Medigap plan, and you want to make changes to your coverage. You can switch to any available Part D plan during the annual open enrollment period, and your medical history will not be a factor. But in most states, your medical history will be a factor if you submit an application for a different Medigap plan.
Louise Norris is an individual health insurance broker who has been writing about health insurance and health reform since 2006. She has written dozens of opinions and educational pieces about the Affordable Care Act for healthinsurance.org. Her state health exchange updates are regularly cited by media who cover health reform and by other health insurance experts.
Footnotes
Tags: Medicare Part A, Medicare Part B, Medicare supplement, Medigap